Development and trends of coronary stents.(HY-industry technical centre)
According to World Health Organization, World Health Statistics 2018 released by WHO, about 17.9 million people worldwide died of cardiovascular disease in 2016, accounting for 44% of chronic non-communicable diseases. Among them, coronary heart disease is a major disease in cardiovascular disease, and percutaneous coronary intervention is one of the current mainstream clinical therapies. As a coronary stent that is essential for percutaneous coronary intervention, it plays a decisive role in the final treatment.
Coronary heart disease and clinical treatment plan
 It is because of the tireless regular pulsation of our heart that maintains the continuous flow of blood in the body’s circulatory system, thus enabling the continuous delivery of oxygen and nutrients to all parts of our body and taking away metabolic waste. It can be said that the heart It is the “engine” that maintains our physical activity. However, the continuous operation of the “engine” also requires the continuous consumption of “fuel” and the discharge of “waste”. How is the “fuel” shipped and how is the “waste” shipped? The answer is “Coronary circulation”. Among them, the “fuel” is transported through the coronary artery, and the “waste” is transported through the coronary vein. It can be seen that the smooth circulation of the coronary circulation plays a vital role in maintaining the normal pulsation of the heart. Once the coronary circulation is blocked, the heart beat will soon stop and cause sudden death.
It is because of the tireless regular pulsation of our heart that maintains the continuous flow of blood in the body’s circulatory system, thus enabling the continuous delivery of oxygen and nutrients to all parts of our body and taking away metabolic waste. It can be said that the heart It is the “engine” that maintains our physical activity. However, the continuous operation of the “engine” also requires the continuous consumption of “fuel” and the discharge of “waste”. How is the “fuel” shipped and how is the “waste” shipped? The answer is “Coronary circulation”. Among them, the “fuel” is transported through the coronary artery, and the “waste” is transported through the coronary vein. It can be seen that the smooth circulation of the coronary circulation plays a vital role in maintaining the normal pulsation of the heart. Once the coronary circulation is blocked, the heart beat will soon stop and cause sudden death.
“Coronary heart disease”, CHD, referred to as coronary heart disease, is a common type of “cardiovascular disease, CVD” that blocks coronary circulation. It refers to myocardial dysfunction and/or organic matter caused by coronary artery stenosis and insufficient blood supply. Sexual lesions. Coronary heart disease originally belonged to “rich disease”, but with the improvement of social living standards, coronary heart disease has gradually “fly into the homes of ordinary people.”
At present, the mainstream clinical treatment programs are divided into three categories: drug therapy, “Percutaneous transluminal coronary intervention, PCI” and “Coronary artery bypass grafting, CABG”.
-
Drug therapy is the basic treatment for coronary heart disease. Once the coronary heart disease is diagnosed, regardless of the degree of coronary artery stenosis, or whether the stent or surgical bypass is implanted, it is necessary to adhere to the oral pro-prognosis for a long time. However, drug therapy is a conservative treatment that only relieves symptoms, stabilizes atheromatous plaque, prevents the occurrence of acute myocardial infarction, and does not substantially solve the problem of coronary artery stenosis, and eliminates or reduces the formed atheromatous plaque.
-
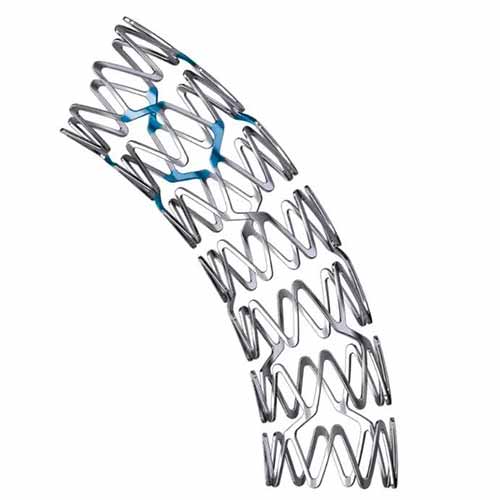
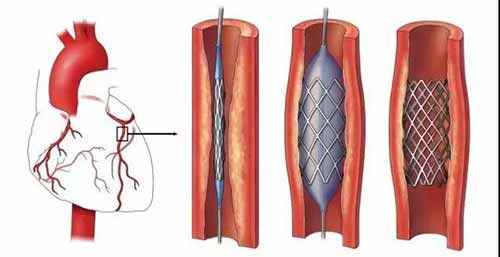
Percutaneous coronary intervention (PCI) usually sends a coronary stent to the coronary artery through the radial or femoral artery. The coronary stent supports the narrow or occluded blood vessels to achieve smooth blood flow, which can effectively improve the myocardium. Blood supply significantly relieves the onset of angina pectoris, improves exercise endurance, and improves quality of life.
-
Coronary artery bypass is the use of the patient’s own Great saphenous vein or other arteries to connect the distal coronary artery to the aorta, so that the narrow coronary artery can be bypassed and blood can be directly supplied to the distal end of the myocardium to improve the myocardium. Blood supply, improve symptoms of angina and improve life treatment.